Renin Angiotensin Aldosterone System (RAAS)
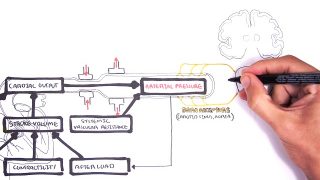
Renin Angiotensin Aldosterone System (RAAS) The renin angiotensin aldosterone system (RAAS) is a hormone system that regulates blood pressure and fluid balance. The juxtaglomerular cells are a group of baroreceptors located in the afferent arterioles of the kidney, which can sense if the blood volume is low, these cells will then secrete renin directly into circulation. […]
Renin Angiotensin Aldosterone System (RAAS)
Other Videos You Might Like:
Subscribe
Login
0 Comments
Newest